Type 1 Diabetes May be REVERSED with OWN
ADULT STEM CELLS
Yes ..there is hope for Diabetes. Researchers have used injections of patients' own stem cells to reverse the course of insulin dependency, reports a research team from the University of São Paulo in Brazil and Northwestern University in Chicago.
The findings, published in the current issue of the Journal of the American Medical Association, exemplify the remarkable gains made by researchers, who are battling a continuously spreading disease that now affects nearly 8% of adults and children. (See the top 10 medical breakthroughs of 2008.)
The research team, led by Dr. Julio Voltarelli of the University of Sao Paulo, is the first to successfully treat these patients with their own stem cells. The group first reported its initial achievement in 2007, with 15 insulin dependent patients who received their own stem cells and No Longer Needed Insulin to control their blood sugar levels.
In the new study, a follow-up of their previous work, Voltarelli and his colleagues detailed the same success with an additional eight patients, and also confirmed that in the majority of them, the stem cell transplant led to an appreciable re-population of functioning insulin-producing beta cells in the pancreas.
"I wouldn't use the word cure," says Dr. Richard Burt, one of the co-authors from Northwestern University. "But it appears we changed the natural history of diabetes. It's the first therapy for patients that leaves them treatment-free — no insulin, no immune suppression.."
Investigate another Stem Cell Release option ..
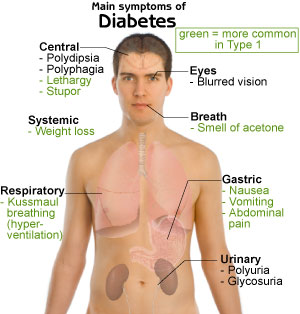
The idea behind the transplant is simple. In type I diabetes, the patient's own immune system turns on the beta cells that produce insulin, the hormone that breaks down the glucose we eat in food. Eventually, the immune cells will virtually eliminate all of the body's beta cells, and glucose levels will start to climb.
Researchers believe that the trigger for this attack lies somewhere within the immune cells, so one possible treatment for the disease may be to wipe out the entire existing immune system and replace it with a fresh one, derived from stem cells without this destructive trait. (See pictures from an X-Ray studio.)
That's the strategy that Voltarelli's team tested. First, they carefully extracted a population of immune stem cells from the bone marrow of each patient. Then each person was treated with radiation, similar to the regimen that cancer patients receive, in order to destroy the immune system. Afterward, each patient received his own stem cells back by injection. The scientists traced blood levels of a protein, C-peptide, that beta cells produce, in order to confirm that whatever remaining beta cells the patient had were now able to grow again and repopulate the pancreas — and produce insulin.
Sure enough, levels of C-peptide rose in 20 of the 23 patients; 12 were able to stay off insulin therapy for three years, and eight needed only intermittent help from insulin treatments during the five-year study period. On average, the patients remained free of insulin injections for 31 months.
That's a milestone insulin dependent patients. Type I diabetes patients are locked in a constant struggle to maintain their body's insulin levels. Since their beta cells no longer produce the hormone on their own, patients must supply it themselves with multiple injections throughout the day and night, or using an insulin pump that dispenses insulin automatically through a permanent tube under the skin. Voltarelli's stem cell strategy provides a life-changing alternative that would take the burden off the patient and put it back where it belongs, on the beta cells.
That's the theory. But some experts point out that, in practice, stem cell transplants are not always a home run. For one, transplantation is a grueling and toxic process in which a portion of the body's tissues — the immune system — is destroyed with dangerous radiation. Then, there is the question of timing. In most cases, patients with type 1 diabetes do not show symptoms of their disease — such as high blood sugar levels — until they have depleted their beta cell population considerably.
Dr. David Nathan, director of the diabetes center at Massachusetts General Hospital, notes that at this point, there may not be enough beta cells remaining to seed a new population of insulin-growing cells, even with an infusion of stem cells to give them a more hospitable environment. "This study shows that it can work, but how long it will work is a question," he says. Previous studies have shown that after an immune cell transplant, beta cells vigorously produce insulin for about six months, and then start to die off, victims of the same immune attack that destroyed their predecessors.
Voltarelli's team, however, has managed to show that the stem cells can give long-lasting beta cells a chance to grow — at least ones that can produce insulin for about three years. Other researchers are pursuing intriguing new stem cell options, including stem cells that can be grown from a patient's own skin, which would eliminate the need for extracting immune stem cells from bone marrow.
"Every door that we open leads to another door," says Burt. "All research is built by sitting on the shoulders of other studies. This trial is something that will contribute to and move the field of stem cell therapy forward." It is, as Burt says, a start.
Investigate a 100% NATURAL Stem Cell option ..No Extractions .. No Injections .. No Surgery
.. .. Now.. Tap HERE & Witness a DIABETES prevention /control Option .. MILLIONS MORE New ,Young STEM CELLS being released from your Bone Marrow, into your Blood Stream, within 60 minutes of ingesting 2 Patented Stem Cell Releaser capsules..
Play the EJ Morris STEM CELL VIDEO Below :
Adult Stem Cells Can Help Prevent DIABETES.. and Help
Control DIABETES ..plus Heart Disease .. Macular Degeneration ..Plus over 70 other Diseases & Health Problems!
Type 1 and Type 2 Diabetics Helped with Stem Cell Treatment
David Rose TIMESONLINE.com UK Edition
Diabetics using stem-cell therapy have been able to stop taking insulin injections for the first time, after their bodies started to produce the hormone naturally again. In a breakthrough trial, 15 young patients with newly diagnosed type 1 diabetes were given drugs to suppress their immune systems followed by transfusions of stem cells drawn from their own blood.
The results show that insulin-dependent diabetics can be freed from reliance on needles by an injection of their own stem cells. The therapy could signal a revolution in the treatment of the condition, which affects more than 300,000 Britons.
People with type 1 diabetes have to give themselves regular injections to control blood sugar levels, as their ability to create the hormone naturally is destroyed by an immune disorder.
All but two of the volunteers in the trial, details of which are published today in the Journal of the American Medical Association (JAMA), do not need daily insulin injections up to three years after stopping their treatment regimes. The findings were released to reporters yesterday as the future of US stem-cell research was being debated in Washington.
Stem cells are immature, unprogrammed cells that have the ability to grow into different kinds of tissue and can be sourced from people of all ages.
Previous studies have suggested that stem-cell therapies offer huge potential to treat a variety of diseases such as Alzheimer’s, Parkinson’s and motor neuron disease. A study by British scientists in November also reported that stem cell injections could repair organ damage in heart attack victims.
The JAMA study provides the first clinical evidence for the efficacy of stem cells in type 1 diabetes. Sufferers of the chronic condition, which normally emerges in childhood or early adulthood, have to inject themselves at least four times a day.
Type 2 diabetes, which tends to affect people later in life, is linked to lifestyle factors such as obesity. There are almost two million type 2 diabetics in Briton, most of whom control their blood-sugar levels with pills or through diet.
The new study, by a joint team of Brazilian and American scientists, found that one of the first patients to undergo the procedure has not used any supplemental synthetic insulin for three years. "Very encouraging results were obtained in a small number of patients with early-onset disease," the authors, led by Julio Voltarelli, from the University of São Paulo in Ribeirão Preto, Brazil. write. "Ninety-three per cent of patients achieved different periods of insulin independence and treatment-related toxicity was low, with no mortality."
Type 1 diabetes occurs when the body’s own immune system malfunctions and destroys the insulin-producing beta cells of the pancreas, causing a shortage in the hormone. By the time most patients receive a clinical diagnosis, 60 to 80 per cent of their beta cells have been wiped out. The disease progresses from this point very quickly, and can result in serious long-term complications including blindness, kidney failure, heart disease and stroke.
Dr Voltarelli’s team hoped that if they intervened early enough they could wipe out and then rebuild the body’s immune system by using stem cells, preserving a reservoir of beta cells and allowing them to regenerate.
They enrolled Brazilian diabetics aged between 14 and 31 who had been diagnosed within the previous six weeks. After stem cells had been harvested from their blood, they then underwent a mild form of chemotherapy to eliminate the white blood cells causing damage to the pancreas. They were then given transfusions of their own stem cells to help rebuild their immune systems.
Richard Burt, a co-author of the study from Northwestern University’s Feinberg School of Medicine in Chicago, said that 14 of the 15 patients were insulin-free for some time following the treatment. Eleven of those were able to dispense with supplemental insulin immediately following the infusion of stem cells and have not had recourse to synthetic insulin since then, he said. "Two other patients needed some supplemental insulin for 12 and 20 months after the procedure, but eventually both were able to wean themselves from taking daily shots, he added." One patient went 12 months without shots, but relapsed a year after treatment after suffering a viral infection, and resumed daily insulin injections. Another volunteer was eliminated from the study because of complications.
The therapy, known as autologous hematopoietic stem cell transplantation, has already shown benefits to individuals with a range of auto-immune diseases such as rheumatoid arthritis, Crohn’s disease and lupus.
"As a research scientist I am always hesitant to speak of a cure, but the initial results have been good and show the importance of conducting more trials," Dr Burt said. In an accompanying editorial in JAMA, Dr Jay Skyler, of the Diabetes Research Institute at the University of Miami, wrote: "Research in this field is likely to explode in the next few years and should include randomized controlled trials, as well as mechanistic studies."
Autologous Nonmyeloablative Hematopoietic Stem Cell Transplantation in Newly Diagnosed Type 1 Diabetes Mellitus Júlio C. Voltarelli, MD, PhD; Carlos E. B. Couri, MD, PhD; Ana B. P. L. Stracieri, MD, PhD; Maria C. Oliveira, MD, MSc; Daniela A. Moraes, MD; Fabiano Pieroni, MD, PhD; Marina Coutinho, MD, MSc; Kelen C. R. Malmegrim, PhD; Maria C. Foss-Freitas, MD, PhD; Belinda P. Simões, MD, PhD; Milton C. Foss, MD, PhD; Elizabeth Squiers, MD; Richard K. Burt, MD JAMA. 2007;297:1568-1576.
Context Type 1 diabetes mellitus (DM) results from a cell-mediated autoimmune attack against pancreatic beta cells. Previous animal and clinical studies suggest that moderate immunosuppression in newly diagnosed type 1 DM can prevent further loss of insulin production and can reduce insulin needs. Objective To determine the safety and metabolic effects of high-dose immunosuppression followed by autologous nonmyeloablative hematopoietic stem cell transplantation (AHST) in newly diagnosed type 1 DM.
Design, Setting, and Participants A prospective phase 1/2 study of 15 patients with type 1 DM (aged 14-31 years) diagnosed within the previous 6 weeks by clinical findings and hyperglycemia and confirmed with positive antibodies against glutamic acid decarboxylase. Enrollment was November 2003-July 2006 with observation until February 2007 at the Bone Marrow Transplantation Unit of the School of Medicine of Ribeirão Preto, Ribeirão Preto, Brazil. Patients with previous diabetic ketoacidosis were excluded after the first patient with diabetic ketoacidosis failed to benefit from AHST. Hematopoietic stem cells were mobilized with cyclophosphamide (2.0 g/m2) and granulocyte colony-stimulating factor (10 μg/kg per day) and then collected from peripheral blood by leukapheresis and cryopreserved. The cells were injected intravenously after conditioning with cyclophosphamide (200 mg/kg) and rabbit antithymocyte globulin (4.5 mg/kg).
Main Outcome Measures Morbidity and mortality from transplantation and temporal changes in exogenous insulin requirements (daily dose and duration of usage). Secondary end points: serum levels of hemoglobin A1c, C-peptide levels during the mixed-meal tolerance test, and anti–glutamic acid decarboxylase antibody titers measured before and at different times following AHST.
Results During a 7- to 36-month follow-up (mean 18.8), 14 patients became insulin-free (1 for 35 months, 4 for at least 21 months, 7 for at least 6 months; and 2 with late response were insulin-free for 1 and 5 months, respectively). Among those, 1 patient resumed insulin use 1 year after AHST. At 6 months after AHST, mean total area under the C-peptide response curve was significantly greater than the pretreatment values, and at 12 and 24 months it did not change. Anti–glutamic acid decarboxylase antibody levels decreased after 6 months and stabilized at 12 and 24 months. Serum levels of hemoglobin
A1c were maintained at less than 7% in 13 of 14 patients. The only acute severe adverse
effect was culture-negative bilateral pneumonia in 1 patient and late endocrine
dysfunction (hypothyroidism or hypogonadism) in 2 others. There was no mortality.
Conclusions High-dose immunosuppression and AHST were performed with acceptable
toxicity in a small number of patients with newly diagnosed type 1 DM. With AHST,
beta cell function was increased in all but 1 patient and induced prolonged insulin
independence in the majority of the patients.
Trial Registration clinicaltrials.gov Identifier: NCT00315133
Author Affiliations: Department of Clinical Medicine, School of Medicine of Ribeirão
Preto, University of São Paulo, Ribeirão Preto, Brazil (Drs Voltarelli, Couri, Stracieri,
Oliveira, Moraes, Pieroni, Coutinho, Malmegrim, Foss-Freitas, Simões, and Foss); Y's
Therapeutic Inc, Bur lingame, Calif (Dr Squiers); and Division of Immunotherapy,
Northwestern University, Chicago, Ill (Dr Burt).
NOTE: There are Natural Stem Cell options to control and beat Diabetes. Investigate Diabetes Stem Cell wellness procedures that Do NOT require ANY Transfusions, NO Extractions or NO Injections.
2 Stem Cell RELEASER Capsules, are proven and documented to mobilize MILLIONS MORE new, fresh adult stem cells from your Bone Marrow, into blood circulation within MINUTES of consumption..
Review these Stem Cell Wellness Options **Click HERE **
Legal Disclaimer:
These articles, products, statements, testimonials, reviews, and videos, have not been evaluated by the Food and Drug Administration. They are for educational and informational purposes only and do not constitute medical advice. The opinions expressed herein are those of the authors and ANY products mentioned or referenced,are not intended to diagnose, treat, cure or prevent ANY disease or illness.
For information on supporting your body’s natural ability to release stem cells, and to take advantage of any opportunities involving More OXYGEN for optimal health ,stem cells and stem cell replacement options …




